December 2022 saw a dramatic increase in the number of cases of meningococcal disease across some of New Zealand’s most vulnerable groups which has prompted a warning from a local vaccinologist.
The following information was written on behalf of GSK by Impact PR (12 December 2022).
According to the latest ESR data, there have been 69 cases of invasive meningococcal disease [during 2022], over a 50% increase in the number of cases compared to the previous year.[1]
Infants and children are most vulnerable to the disease, in particular Maori and Pasifika who made up 90% of all cases in children aged under five this year.[1] Teens and young adults are also at increased risk, making up 28% of cases in people under 30 years of age.[1]
Across the regions, Bay of Plenty and Otago/Southland have also been disproportionately affected, each recording the country’s highest rates of the disease and accounting for almost a quarter (23%) of cases in 2022. Northland, West and South Auckland made up a further 30% of cases.[1]
Meningococcal disease is an uncommon but life-threatening bacterial infection causing two serious illnesses: meningitis (an infection of the membranes that cover the brain) and septicaemia (blood poisoning).[2] Even with prompt medical care, around one in every ten patients who contract the disease will die, and up to one in five survivors will have permanent disabilities, such as brain damage, amputated limbs and hearing loss.[3][4][5]
There are several types or serogroups of meningococcal bacteria including groups A, B, C, W and Y. The most common in New Zealand is meningococcal group B, which made up 80 percent of cases [in 2022]. *[6][7]
Meningococcal B vaccine
The meningococcal B vaccine will be funded as part of scheduled childhood immunisations from 1st March 1 2023, with a catch-up programme for the next two and a half years to provide vaccination for all children under the age of five.
Meningococcal B vaccination will also be funded for people aged 13-25 in close-living situations such as hostels, boarding schools, halls of residence and the military, with a one-year catch-up programme for young people already living in closed living environments.
This vaccine was previously only funded for those with reduced immune function or close contacts of a meningococcal case.
It is estimated that around 300,000 Kiwis will be eligible during the catch-up period and around 60,000 new infants and young people each year following.[8]
A timely reminder to be vigilant
University of Auckland Associate Professor Dr Helen Petousis-Harris says the rise in cases is a timely reminder to parents of infants and teens to be vigilant in identifying the early stages of the disease. She says there is often confusion around protection status with parents who may think their children are already covered under the childhood immunisation schedule.
“Infants are a high-risk group because their immature immune system makes it easier for the bacteria to invade their bloodstream and they have not had time to develop natural immunity. Children who attend pre-school or daycare are also at greater risk,” she says.
“Meningococcal disease can have a debilitating impact on patients and their whanau. It may loiter around in the community without any cases and then all of sudden you can have a surge and an outbreak. We have been concerned for a long time about the potential for New Zealand to experience a significant outbreak,” she says.
New Zealand has a higher rate of invasive meningococcal disease compared with other developed countries, and the rate of disease has been increasing since 2014.[9][10][11][12]
“The new data is a timely reminder that meningococcal disease can be circulating in the community, and we must be vigilant in protecting against it and recognising the symptoms. Meningococcal disease can develop rapidly usually starting with a fever, vomiting, headache and a general feeling of being unwell. However, this can progress very quickly to a rash, pain in the limbs, cold hands and feet, neck stiffness, confusion and aversion to bright lights,” she says.[13][14]
Under the current Pharmac funding framework, there will still be a cohort of young adolescents who are at increased risk but will not meet the criteria for funded access – including secondary and tertiary students not in close living conditions.
Brett Marett, Medical Director at GSK NZ says although uncommon, invasive meningococcal disease can have high mortality and profound, life-long effects.
“Rates of meningococcal disease in New Zealand are high, double the cases compared to Australia and 25 times higher than what is reported in the United States.”[15][16][17]
“With a limited catch-up window, we encourage all parents and health care providers to prioritise vaccinating those at risk against meningococcal B. For children who have begun their childhood vaccinations, and young people, this means that they may need to schedule additional appointments to receive their vaccine,” he says.
(Please see below for references)
The following information was written by Kidspot NZ
What is meningococcal disease?
Meningococcal disease is a bacterial infection that can result in two serious illnesses: meningitis (infection of the membranes covering the brain) and septicaemia (blood poisoning).
The bacteria are passed from person to person through coughing, sneezing, kissing, sharing utensils, toothbrushes, pacifiers, etc. Good hygiene practices are essential including covering your mouth and nose when sneezing or coughing, and washing and drying hands to help prevent the disease spreading.
It can be treated with antibiotics but needs to be caught early.
Know the symptoms
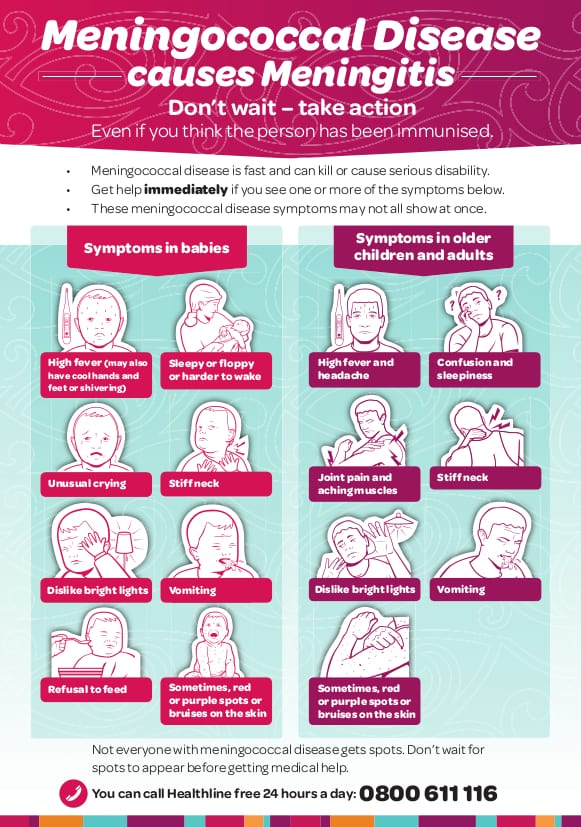
Meningococcal disease can progress into a very serious medical emergency extremely quickly. Symptoms are often similar to flu, ie high fever and muscle aches. The well-known meningitis rash is not always present. Refer to the symptom checker below for more information. If in doubt, take action and seek medical advice urgently.
For a printable version of the symptom checker above, click here.
This article was written by Julie Scanlon, Editor for Kidspot NZ. Sources include Ministry of Health.
Read more on Kidspot:
References:
[1] Provisional Meningococcal disease 1 Jan 0 30 Nov 2022. Data source: Episurv as of 7 Dec 2022 and Special Pathogens Unit
[2] Ministry of Health website. Meningococcal disease (including meningitis.) Summary Tab. Available here: Accessed 17 October 2018
[3] Thompson MJ, et al. Lancet 2006; 367(9508): 397–403.
[4] Immunisation Advisory Centre. Bexsero: A vaccine to protect against Meningococcal group B disease Fact Sheet. Available here: Accessed 15 September 2018
[5] Rosenstein NE, et al. N Engl J Med 2001; 344(18): 1378–88
[6] Provisional Meningococcal disease 1 Jan 0 30 Nov 2022. Data source: Episurv as of 7 Dec 2022 and Special Pathogens Unit
[7] Ministry of Health website. Meningococcal disease (including meningitis.) Summary Tab. Available here: Accessed 29 August 2020
* of those cases that could be typed
[8] Pharmac proposal. Available here.
[9] The Institute of Environmental Science and Research. Meningococcal Disease Report September 2019. Available here: Accessed 28 October 2019.
[10] Australian Government Department of Health. Invasive Meningococcal Disease National Surveillance Report Quarter 4 2018. Available here: Accessed 7 November 2018.
[11] CDC. Enhanced Meningococcal Disease Surveillance Report, 2017. Available here: Accessed 1 April 2019.
[12] England ref: Public Health England. Invasive Meningococcal Disease in England: annual laboratory confirmed reports for epidemiological year 2017 to 2018. Available here (PDF): Accessed 1 April 2019.
[13] World Health Organization (WHO), 2018. Meningococcal meningitis Fact sheet no 141. Available here: Accessed July 2019.
[14] Thompson MJ et al. Lancet. Clinical recognition of meningococcal disease in children and adolescents. 2006;367:397-403
[15] New Zealand Public Heath Surveillance, 2019. Environmental Science Research, Invasive Meningococcocal Disease Report, 10 January 2019.
[16] Australian Government Department of Health. Invasive meningococcal disease national surveillance report. Q4 2018. Accessible here.
[17] Centers for Disease Control and Prevention (CDC), 2017. Enhanced meningococcal disease surveillance report, 2017. Accessible here (PDF).








A very useful fact sheet enclosed in this article. Its one I will be sharing with friends and family.
Thanks for this information. It’s hard enough to say the name of this disease. It’s a good reminder to do the things we take for granted at times like washing our hands when we are rushing. It’s starts with simple steps and always making sure we follow good hygiene practices. Like they say prevention is better than cure.
Wowee scary facts with this story. Unbelievable that there were 29 cases nationwide resulting in some deaths also around the country. I remember a young child that was in the same small town as me when I was a child he caught it and lost fingers. Was very close to not surviving as he was so young. Real little fighter and a mother down there also didn’t make it. It’s a very bad virus. When it attacks someone it does just that.
It is a very scary disease and I love most Mum like to know the symptoms and feel its better to be safe than sorry. It is interesting though as my daughter had it but by the time my son was due they had stopped it. I was told it was stopped because it didn’t seem to be affective at stopping people from getting it?
My eldest got the vax when it was free and I think she had 3 boosters in top of the other. By the time my youngest came around it wasn’t in the free vax mix. It is a really serious illness and I’m also always looking for a rash if they have a fever. I guess miss 11 being vax is why they have that middle non-eligible age group. Because those kids would have potentially had the free coverage already.
P.S please take the time to sign the petition which is almost at 1000 signatures:
https://www.parliament.nz/en/pb/petitions/document/PET_82261/petition-of-nicole-moana-full-nationwide-funding-for?fbclid=IwAR1uViOGh0oBI7RRi2xJA9hT5dX-sJCgc-648SCy1eTIFCqIbOc-mS9fg1g
Unfortunately family friends lost their 19 year old daughter to this awful disease just recently 🙁 They have campaigned to get the vaccine available to all vulnerable groups in the hopes that it will spare future unnecessary deaths amongst our people.
I think the free vaccines are a great idea. It is a truly scary disease – one of the parents at my daughters school ended up in hospital with it!! I’m always on the look out for symptoms when my daughter gets ill
This is really scary, it is so fast! Everytime my kids come down with a fever it watch for the symptoms of meningococcal disease. A few weeks ago my youngest became very sick with a fever and developed a rash, we went straight to the doctors! Luckily it was a virus that he recovered from quite quickly but it was concerning!
Thanks for this I just printed of the symptom checker as it’s such a hard one to diagnose. We live in the South Island and my kids fall between the vaccination groups so would be unable to be vaccinated if it came to the South Island without paying for it which sucks. I’m keeping a close eye on this as it is a real concern.
Thank you for sharing this and the symptoms to look for as well as prevention. This article hits quite close to home as a really good friend lost her son to septicemia and it happened suddenly and without warning, the hospital sent them home on first visit and by the time he went in again it was too late… Need to be vigilant always!!