Welcome to a whole new world of words and acronyms! The journey through conception, pregnancy, labour and birth can be like learning a new and strange language.
The best way to take the mystery out of the process is to know what everything means so we have put together a handy glossary for you.
Conception
Cervix – the lower part of the uterus
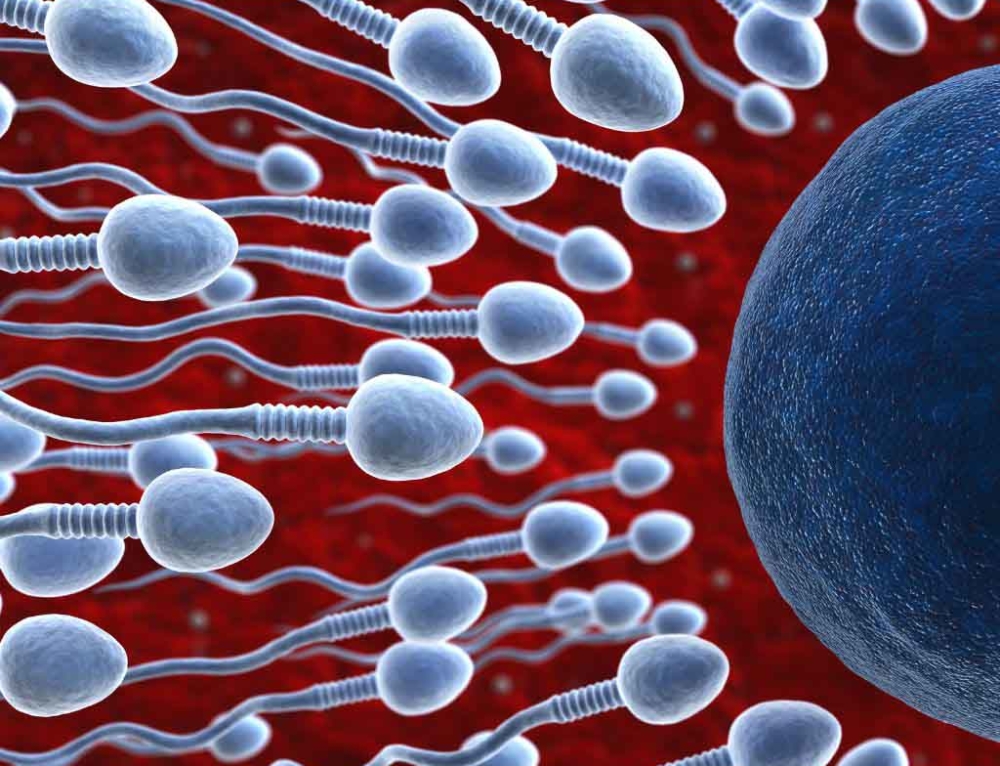
Conception – occurs when sperm penetrates the outer layer of an egg and fertilises it
Egg (or ovum) – produced by ovaries
Embryo – the first 2-8 weeks of a baby’s growth after conception
Fallopian tube(s) – tubes that transport eggs from the ovaries to the uterus
Fertilise – when an egg and sperm join and the embryo begins to grow. When an egg is fertilised, conception occurs.
Folic acid – also known as folate, is a water-soluble B-group vitamin. Like all water-soluble vitamins, folic acid is not stored in the body and must be replenished each day. Folic acid is vital for the formation of red blood cells, DNA synthesis and for protein metabolism, and for the prevention of neural tube defects in the developing foetus during early pregnancy.
Foetus – the baby from the end of the embryo stage to birth
IUI – Intra Uterine Insemination. Where sperm is placed directly into the uterus.
IVF – In Vitro Fertilization. When eggs from ovaries and sperm are fertilised in a laboratory or similar and then the embryos are then transferred into the uterus.
Motility – how well sperm moves once ejaculated
Morphology – the shape and structure of a sperm. A healthy sperm’s morphology includes an oval head and a long tail to propel it forward.
Ovary(ies) – organs that store eggs and release one each menstrual cycle.
Semen – when ejaculation occurs, a mix of sperm and semen is ejected. Semen helps the sperm on its journey to the egg.
Sperm – the male reproductive cell. When it penetrates an egg and fertilises it, the embryo begins to grow
Uterus – also known as the womb. Where the baby grows and develops.
Vagina – the internal canal that connects the vulva to the uterus and cervix
Vulva – the external female sex organs. Includes the clitoris and labia
Pregnancy
Amniotic fluid – the fluid that surrounds the foetus inside the amniotic sac it is growing in, in the uterus
Amniotic sac – the membrane that the foetus is growing in, inside the uterus
Ectopic pregnancy – when the foetus begins to grow in the fallopian tube rather than the uterus. This pregnancy must be surgically removed.
Edema – swelling of ankles, legs, feet and hands
Estimated Due Date (EDD) – date the baby is due
Gravida – the number of pregnancies prior to the current one
Incompetent cervix – where the cervix opens too soon. Can cause miscarriage or early birth. Can be treated.
Term (or full term) – a baby born between 37 and 42 weeks or is over 2500 grams
Trimester – the pregnancy is divided into trimesters. The first is up to 12 weeks, the seconds between 13 and 28 weeks and the third is the time span beyond 28 weeks.
Fundal height – the measurement of the pregnant belly from the top of the pubic bone to the top of the womb. It is used to help establish how well the baby is growing
Fundus – the top of the uterus
Geriatric Pregnancy – if the pregnant person is over 35 years old, their pregnancy is known as ‘geriatric’
Gestation – essentially the time the baby is in the womb. Synonymous with pregnancy
Gestational age – the age of the fetus from the date of the last menstrual period
Gravida – the medical term for a pregnant person
Human chorionic gonadotropin (hGC) – hormone produced during pregnancy. This is what is detected to give a positive urine-based pregnancy test
Lead Maternity Carer (LMC)- midwife or specialist doctor who looks after you throughout the pregnancy and through to around 6 weeks
Linea nigra – a dark line that may appear on the skin down the centre of the abdomen during pregnancy caused by hormonal changes.
Midwife – a person who has completed training to care for women during their childbearing years and attend to low-risk pregnancies and births.
Pelvic floor muscles – the muscles that support the uterus, bladder, vagina and rectum
Pelvis – the abdomen between the hip bones
Placenta – grows in the uterus and attaches to the uterine wall. The baby is connected to the placenta with the umbilical cord and get all its nutrients and oxygen from it. This will be delivered separately after the baby is born.
Primigravida – first pregnancy
Quickening – when the first movements of the fetus can be felt
Scan – ultrasound
Stretch marks (striae) – the marks left behind when the skin stretches
Pregnancy and birth
Afterpains – contractions or cramps that signal your uterus return to its pre-pregnant size and shape
Birth centre – a homier alternative to a hospital, equipped to care for women experiencing a low-risk pregnancy.
Birth defect – any defect that is present at birth – caused by genetic defect or non-genetic prenatal events
Bloody show / mucous plug – as labour approaches and the cervix begins to dilate, the thick plug of mucus that is sitting in the cervix can come out.
Breech – in about 3-4% of pregnancies, the baby approaches full-term by presenting in breech position meaning it is bottom or feet down, rather than head down.
Caesarean (c-section) – the delivery of a baby via a surgical incision to the abdomen.
Contractions – tightening of the uterus. When in labour, the force of the contractions help the baby progress down the birth canal.
Cord prolapse – premature expulsion of the umbilical cord in labour before the fetus is delivered. Needs urgent medical attention
Crowning – when the baby’s head appears at the vaginal opening shortly before delivery.
Dilation – the process during the first stage of labour where the cervix widens to 10 centimetres
Dysfunctional labour – failure to progress in a clinically normal pattern of labour
Effacement – during the first stage of labour, the cervix shortens. This process is called effacement
Episiotomy – a surgical incision made to the perineum during the birthing process to enlarge the vaginal opening.
False labour – when labour does not progress and then eventually stops
Foetal distress – warning signs indicating fetal hypoxia (deficiency in amount of oxygen reaching foetal tissues)
Forceps – large tongs which are occasionally used to help assist the delivery of a baby
Induced labour – the use of drugs and/or procedures are used in an attempt to start labour.
Labour – the onset of regular, progressive contractions until the birth of a baby.
Moulding – where the baby’s skull sutures overlap and the head shape temporarily changes to negotiate the journey through the mother’s pelvis.
Natural birth – generally refers to childbirth without pain relief (anesthesia or analgesia) but may alternatively be used to describe a vaginal delivery rather than a cesarean birth.
Precipitous labour – very quick labour and delivery, which lasts less than three hours from beginning to end.
Presentation – the part of the foetus that enters the birth canal first. Some presentations include variations of cephalic (head), breech (bottom, legs or feet) or shoulder.
Prolonged labour – labour lasting more than 20 hours. There are many reasons why labour may not progress more quickly, and this does not always signify a problem.
Transition – the phase of labour just before the pushing stage. During transition, contractions become very strong, and often their duration and frequency are less predictable.
Umbilical cord – baby’s lifeline connecting the foetus at its abdomen (the eventual tummy button) and the placenta, and giving passage to the umbilical blood vessels. The placenta transports oxygen and nutrients from the placenta to the baby. Needs to be cut after birth.




Leave A Comment
You must be logged in to post a comment.